Oncolytic Virotherapy
The idea of using a virus for cancer treatment or oncolytic virotherapy is not a new idea. In the 1940s scientists conducted animal studies using viruses to treat tumors. Doctors in the 1950s observed that cancer patients that were stricken with viral infections or recently vaccinated experienced improvement in their condition. It was believed that the infections or vaccinations triggered an immune response that increased the production of interferon and tumor necrosis factors, or TNFs.
Interferons are large molecules released by cells infected with viruses, bacteria, parasites and tumors to interfere, hence their name, with virus reproduction and to trigger responses from immune cells. Interferons activate natural killer white blood cells and large white cells called macrophages that attack and destroy the invading organisms and cancer cells. Interferon promotes the production or molecular complexes that attach to viral, bacterial, parasite, and tumor cells so they are more quickly and effectively attacked by killer white cells. TNFs causes destructive changes in cell walls and causes foreign or tumor cells to burst and die
Despite the potential for viral therapy of cancer in these early years, it required the present advances in technology to achieve a real possibility. Precisely, it required our present ability to genetically modify organisms like viruses and safely use them to target cancer cells. The viruses are modified to prevent their normal ability to cause disease and genetically altered to produce interferon or other anti-cancer molecules.
Preliminary Study in Dogs
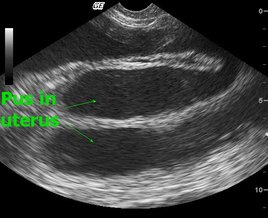
The abstract was based on a small study intended to evaluate the safety and effectiveness of a new oncolytic virus. The group was made up of of seven dogs suffering from various cancers (lymphoma, malignant melanoma and multiple myeloma). The researchers used a novel virus for their study; they used a modified vesicular stomatitis virus that causes oral, udder, and hoof ulcers in cattle. Although seldom fatal, the disease causes inappetence and decreased milk or meat production [in cattle]. It can also infect horses and pigs, and rarely, sheep, goats, and llamas. Because of its effect on agricultural production, vesicular stomatitis is a diagnosis that requires mandatory reporting to federal and state animal health officials.
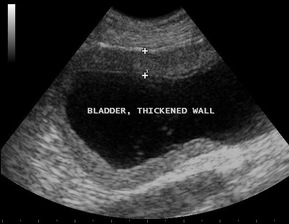
The virus was also modified to produce human or canine interferon. Three dogs received the human form and four dogs received the canine form. The abstract reported measurable improvement but did not specify the type and extent of the improvements except for the production of neutralizing antibodies within 7-10 days after viral administration. Side effects were minimal and included reversible changes in liver enzymes, fever, and urinary tract infection. Virus was not shed in the urine or saliva. These limited side effects are comparable or even fewer than those expected with radiation or chemotherapy.
This is a small study and rightly titled as preliminary. It has yet to be published so critical evaluation is still not available. Clearly, much more study is required for this type of treatment. What is exciting is that this is one of many new potential treatments for cancer in pets. Advanced cancer treatment in the last decade has changed how the diagnosis is now viewed. Rather than an immediate death sentence, cancer can now be better managed as a chronic disease much like kidney and heart conditions. These new treatments offer greater treatment flexibility and potentially an improved quality of life.





 RSS Feed
RSS Feed
