Findings
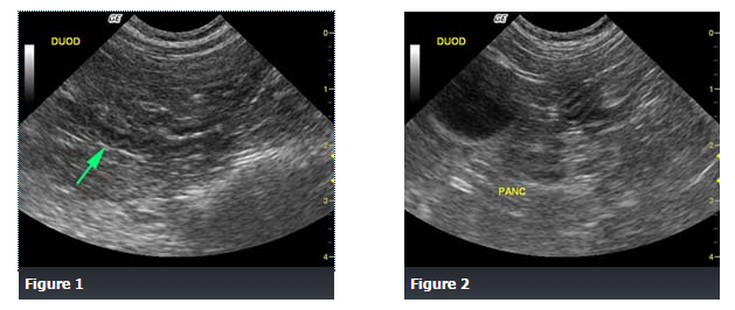
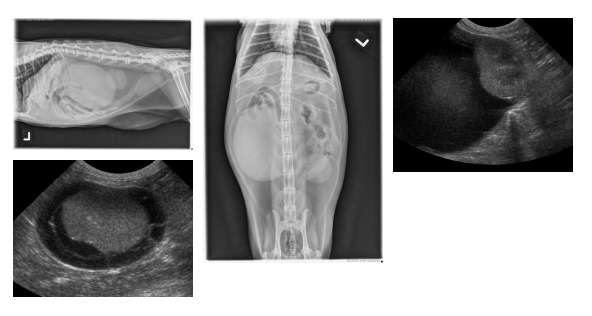
Abdominal ultrasound revealed a spastic duodenum (Figure 1), an enlarged, irregular, hypoechoic pancreatic body (Figure 2) and a hypoechoic left pancreatic lobe (Figure 3), as well as hyperechoic surrounding mesentery which surrounded the body and left pancreatic lobe.
Differential Diagnosis
Pancreatitis
Acute gastroenteritis
Inflammatory bowel disease
Gastrointestinal obstruction
Peritonitis
Acute renal failure
Diagnosis
Pancreatitis
Discussion
The cat responded well to medical management of pancreatitis with intravenous fluid therapy, famotidine and pain medication.
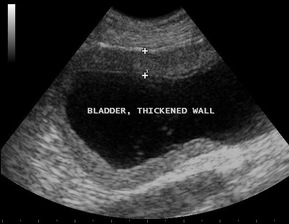
Pancreatitis is inflammation of the pancreas and it can be acute (sudden) or chronic (recurrent) in nature. It is associated with a range of clinical signs that vary in severity, often overlapping with signs of acute gastroenteritis, inflammatory bowel disease, gastrointestinal obstruction, peritonitis, or acute renal failure. Therefore, ultrasound is a very useful diagnostic tool to help differentiate among these similar presenting conditions.
The cause of pancreatitis in dogs and cats is usually unknown.
Source: soundvet.com

 RSS Feed
RSS Feed
